REVIEW: What Adaptive Changes in Hemagglutinin and Neuraminidase Are Necessary for Emergence of Pandemic Influenza Virus from Its Avian Precursor?
A. S. Gambaryan1* and M. N. Matrosovich2
1Chumakov Institute of Poliomyelitis and Viral Encephalitides, Poselok Institute of Poliomyelitis, 142782 Moscow, Russia; fax: +7 (495) 841-9330; E-mail: al.gambaryan@gmail.com2Institute of Virology, Philipps University, Hans-Meerwein-Str. 2, Marburg 35043, Germany; fax: 06421-28-68962
* To whom correspondence should be addressed.
Received January 20, 2015; Revision received March 13, 2015
Wild ducks serve as the primary host for numerous and various influenza type A viruses. Occasionally, viruses from this reservoir can be transferred to other host species and cause outbreaks of influenza in fowl, swine, and horses, as well as result in novel human pandemics. Cellular tropism and range of susceptible host species are determined by interaction between virus and receptor molecules on cells. Here we discuss modern data regarding molecular features underlying interactions of influenza viruses with cellular receptors as well as a role for receptor specificity in interspecies transmission. By analyzing the earliest available pandemic influenza viruses (1918, 1957, 1968, 2009), we found that hemagglutinin reconfigured to recognize 2-6 sialic acid-containing receptors in the human upper airway tract together with altered enzymatic activity of neuraminidase necessary for maintaining functional balance with hemagglutinin are responsible for effective spread of influenza viruses in human populations. Resistance to low pH also contributes to this. Thus, a combination of such parameters makes it possible that influenza viruses give rise to novel pandemics.
KEY WORDS: influenza virus, receptor specificity, pandemicDOI: 10.1134/S000629791507007X
Abbreviations: HA, hemagglutinin; NA, neuraminidase.
HOW DO INFLUENZA PANDEMICS ARISE?
Wild waterfowl, primarily ducks and seagulls, create the main natural reservoir of influenza viruses, which replicate in their intestines and cause mainly asymptomatic infection to be preferentially transmitted via fecal-oral route through contaminated water [1]. During evolution in the birds, influenza A viruses diverged into 16 antigenic subtypes of hemagglutinin (HA) (H1, H2, H3, etc.) and nine antigenic subtypes of neuraminidase (NA) (N1, N2, etc.). Protection from being infected with influenza viruses is mainly linked to production of anti-HA antibodies, and to lesser extent – anti-NA antibodies, so they do not protect against infection with unrelated viral subtype. Waterfowl influenza viruses are able to infect other species of birds and marine and terrestrial mammals, in particular, seals, horses, and swine. Rarely, influenza viruses adapt to a new host and continue to circulate in it by making a stable evolutionary lineage. It is generally accepted that all lineages of influenza viruses from domestic fowl and mammals originated from the waterfowl viruses.
Very rarely, influenza viruses from animals can infect humans. In exceptional cases, a virus obtains mutations allowing it to effectively replicate in humans. If a human population lacks anti-HA immunity against a novel influenza virus, it can result in a global epidemic (pandemic). Influenza pandemics have attacked humankind at least over the last 500 years. Three influenza pandemics occurred in the twentieth century. It seems that H1N1/1918 virus was transmitted from fowl as a whole entity containing all genes encoding internal and surface proteins [2, 3]. It caused a catastrophic epidemic known as “Spanish” pandemic that killed more than 20 million people.
Two other pandemics were caused by reassortant H2N2/1957 and H3N2/1968 influenza viruses, which preserved the majority of genes coding for internal proteins from the previous human viruses [1, 4]. Pandemic H2N2/1957 virus displaced from circulation a previous influenza A virus, as did H3N2/1968 virus with regard to evolutionary lineage of 1957 influenza viruses. Influenza viruses of 1918-1957 unexpectedly returned to circulation in 1977. Importantly, the virtually full nucleotide sequence of this virus matched to the 1952 influenza viruses, indicating that it was preserved in a “frozen” state. Thus, this pandemic was perhaps due to the escape of a laboratory virus strain. The last influenza pandemic occurred in 2009 when H1N1 swine subtype was transmitted to humans.
Among the other things, knowing the mechanisms used by fowl influenza viruses to adapt to humans is necessary for predicting and preparing for potential novel pandemics.
HOW DOES A PANDEMIC INFLUENZA VIRUS EMERGE?
It is generally accepted that such adaptation may require a changes in many viral genes. However, adaptation of HA and NA plays a special role. Owing to a capacity for reassortments, a novel virus can replace a majority of unadapted avian genes for preadapted genes from human viruses as occurred, for example, with pandemic 1957 and 1968 influenza viruses. At the same time, by definition any pandemic virus must contain avian precursor HA, which is necessary for effective spread of a novel virus in the human population.
HOW DOES INFLUENZA VIRUS INFECT CELLS?
The main function for HA and NA is to interact with cellular receptors. The top part of both proteins contains the active center, which is responsible in HA for binding to a terminal sialic acid (Sia) of the cellular glycan receptor, whereas in NA it is represented by a catalytic site that cleaves terminal sialic acid from a galactose residue. Such degradation facilitates budding of new virions off the parent cell and contributes to their passage through the mucin barrier covering epithelial cells [5].
Infection is triggered when virus attaches to sialyloligosaccharide residues on the cellular glycoproteins and gangliosides [6] that are expressed on the target cells and generally can serve as receptors for influenza viruses [7]. By the 1990s, it was shown that receptor specificity of avian influenza viruses differed from that for human viruses, so that the former preferentially bind to the terminal Siaα2-3Gal-residues, whereas the latter possess higher affinity to Siaα2-6Gal-containing receptors. Notably, HA from human pandemic influenza viruses that originated from avian viruses differed from the parental avian HAs only by several amino acid positions and already possessed altered receptor specificity [6, 8-12].
WHICH INFLUENZA VIRUSES CAN INFECT HUMAN RESPIRATORY
EPITHELIUM?
Until 2004, it was predominantly viewed that human respiratory epithelium is mainly represented by glycans containing Siaα2-6Gal-residues [13]. Inability of influenza viruses with Siaα2-6Gal-specificity to infect humans was explained by the fact that Siaα2-6Gal-containing receptors dominate on the human respiratory epithelium, whereas human mucins preferentially possess Siaα2-3Gal-groups, so the viruses are unable to find appropriate receptors and become profoundly inhibited by mucins [14]. However, this theory came into conflict with the capacity of H5N1 influenza viruses to successfully infect humans despite their Siaα2-3Gal-specificity [15-17].
Examination of human respiratory epithelium cell cultures in experiments with lectins, as well as investigation of their ability to bind to and to be infected with avian and human influenza viruses, demonstrated that ciliated epithelial cells possess significant numbers of Siaα2-3Gal-residues and can become effectively infected by avian viruses, whereas human viruses mainly infect secretory cells with more pronounced expression of Siaα2-6Gal-bearing receptors [18]. This study showed that differences in pathogenicity and replication of human and avian influenza viruses in humans might be related to their various cellular tropisms.
Similar conclusions were made by Thompson et al. [19], who confirmed that human airway epithelial cultures contained both Siaα2-3Gal and Siaα2-6Gal-receptors, with the former being better represented on ciliated, and the latter on non-ciliated cells. Avian influenza virus exclusively replicate in ciliated epithelial cells, whereas contemporary human H3N2 influenza virus preferentially replicated in non-ciliated cells.
Both types of receptors (Siaα2-3Gal- and Siaα2-6Gal-terminated) were found on the surface of human bronchial epithelial cells using MAA and SNA lectins [20].
AIRBORNE TRANSMISSION – A CRITICAL CONDITION FOR
INFLUENZA PANDEMIC
To summarize, we mention that: 1) human airway epithelium contains receptors for both human and avian influenza viruses, and 2) both types of viruses are able to replicate in the human airway tract. However, viruses recognizing Siaα2-3Gal-receptors would never stay in the human population, and development of pandemic influenza viral strain requires changes in its receptor specificity. It is well accepted that acquisition of airborne human-to-human transmission by virus is a critical condition for development of human pandemic influenza strain. During recent years, a number of studies have been published aimed at investigating this issue in ferrets as a course of influenza resembles that in humans, and they contain sialoglycoconjugates mainly corresponding to that in humans. Modern human influenza viruses are effectively transmitted via the airborne route and demonstrate good transmissibility in the ferret model. However, H5N1 viruses, being highly pathogenic to ferrets, similarly to birds and humans, are not transmitted via the airborne route [21].
So, why do viruses recognizing Siaα2-6Gal-terminated receptors better transmitted via the airborne route than viruses biding to Siaα2-3Gal-receptors? Partially, this is related to the distribution of the cells bearing Siaα2-3Gal and Siaα2-6Gal in the airway tract.
DISTRIBUTION OF Siaα2-6Gal- AND Siaα2-3Gal-TERMINATED
RECEPTORS IN THE HUMAN AIRWAY TRACT
Shinya and Kawaoka showed that Siaα2-6Gal-terminated receptors are predominantly expressed on human cells from the upper airway tract, and their amount gradually declines as follows: nasal epithelium > paranasal sinuses > trachea > bronchi > bronchioles. Siaα2-3Gal-terminated receptors were found on cuboid bronchiolar cells as well as cells lining the alveolar walls. Human influenza virus binds to bronchiolar cells, but not to alveolar cells, whereas avian viruses including H5N1 influenza virus bind better to alveolar cells [22]. It was demonstrated that in tissue samples obtained from a sick patient, replication of H5N1 influenza virus in the airway tract was limited to lungs, primarily pneumocytes [23].
Gu et al. examined the distribution of Siaα2-3Gal and Siaα2-6Gal expression in the human airway tract using biopsy samples. Alveolar lung cells were found to express Siaα2-3Gal at the highest level, which declined upwards along the respiratory tract, whereas expression of Siaα2-6Gal had the opposite pattern [24].
The capacity of H5N1 influenza viruses to replicate in various parts of the human respiratory tract was also studied by Nicholls et al., who infected biopsy samples in organ culture with avian H5N1 and human H3N2 influenza viruses and demonstrated that both viruses perfectly replicated in tissue samples from nasopharyngeal, adenoid, and tonsillar areas [25].
Riel et al. compared binding of H5N1 influenza virus to the cells from the lower respiratory tract. In humans, this viral strain preferentially bound to type II pneumocytes, alveolar macrophages, and non-ciliated cuboid cells from terminal bronchioles. While moving upwards towards trachea, such binding became attenuated. It was assumed that the location of the virus exclusively within the lower airway tract was responsible for inability of H5N1 influenza viruses to be transmitted between people via the airborne route [26].
Importantly, it was concluded that the location of the target cells in the human airway tract that bind human and avian influenza viruses does not coincide. Human influenza viruses primarily target the upper airway tract, whereas avian viruses target terminal bronchioles and lung alveoli. The main factor responsible for obtaining capacity to airborne transmission is considered to be a readjustment of the viral receptor-binding site to recognize Siaα2-6Gal-terminated receptors, as the upper airway tract is enriched with them.
WHAT CHANGES IN STRUCTURE OF HEMAGGLUTININ RETARGET INFLUENZA
VIRUS TO RECOGNIZE NOVEL RECEPTORS?
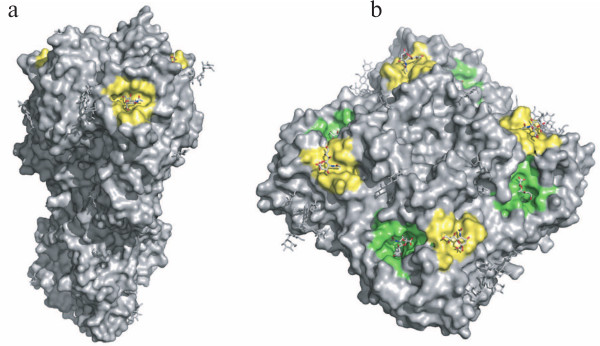
A special region located on the top of HA known as the receptor-binding site is responsible for its binding to the receptor. Cristal structures of H1, H3, H5, H7, and H9 of HA done in complex with oligosaccharide demonstrated that sialic acid is immersed into the cavity on the protein surface with walls being lined up with conservative and semiconservative amino acids (Fig. 1) [27-32]. The bottom of the receptor-binding site I composed of absolutely conserved amino acids such as Trp153, His183, and conservative Tyr98 residue excepting subtype 16. The walls comprise absolutely conservative Gly134 residue, Glu190, Leu194, Gly225, Gln226, and Gly228 that are conservative for all duck influenza viruses, and semiconservative Thr155 and Ser227. Such structure of the receptor-binding site provides optimal binding of sialoglycoconjugates bearing Siaα2-3Gal-terminated residues. The affinity of duck influenza viruses to Siaα2-3Gal-group is higher than to free α-form of sialic acid, which shows energetically advantageous interactions with galactose that is bound with sialic acid via a 2–3 bond [10].
Fig. 1. Hemagglutinin trimer (a) and neuraminidase tetramer (b) of influenza A viruses. The receptor-binding site of HA and hemadsorption site of NA as well as the catalytic site of neuraminidase are highlighted in yellow and green, respectively. This figure was made using the 1MQM and 1W20 crystal structures (Protein Data Bank).
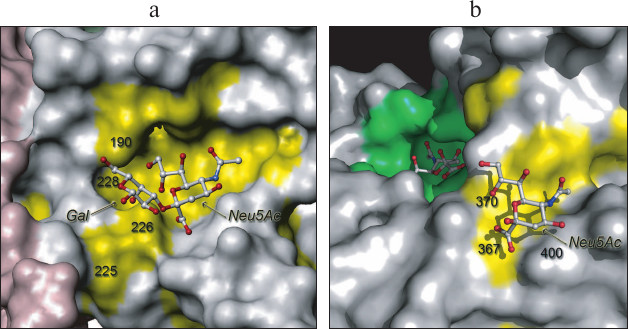
The four last influenza pandemics demonstrated two mechanisms for acquiring capacity to recognize Siaα2-6Gal [12]. Mechanism 1 was based on Gln226/Leu and Gly228/Ser substitutions (Fig. 2), which independently emerged in H2N2 and H3N2 influenza subtypes that resulted in the 1957 and 1968 pandemics. Interestingly, the same two substitutions were also found in H4N6 swine isolate, whose receptor specificity completely matched that of the earlier H3N2 subtype known as A/Aichi/2/68 [33].
Fig. 2. Changes in receptor-binding site of HA (a) and hemadsorption site of NA (b) during development of pandemic influenza viruses. Conservative amino acids found in the receptor-binding site of HA and the hemadsorption site of NA from the majority of avian influenza viruses are highlighted in yellow. The fragment of Neu5Ac2-3Gal inside the receptor-binding site of HA as well as the Neu5Ac residue inside the hemadsorption site of NA are depicted as ball-and-stick models. Constant amino acids in HA and N2 NA from avian influenza viruses that change in H1N1, H2N2, and H3N2 pandemic influenza viruses are enumerated.
Mechanism 2 underlying recognition of 2-6 sialylgalactose receptors was employed in H1N1 viruses (Fig. 2). All five sequenced human H1N1 1918 influenza viruses were found to bear Glu190Asp substitution. In case this amino acid substitution was alone, such viruses exhibited a mixed α2-6/α2-3-receptor specificity compared to “consensus” avian influenza viruses. Viruses bearing an additional Gly225Asp substitution lost capability to bind Siaα2-3Gal-terminated receptors and possessed the highest affinity to the extended trisaccharide region 6′-sialyl-N-acetyllactosamine (6′SLN) [34-36]. Mutation of the amino acid at position 190 was also found in all H1N1 and H9N2 swine influenza viruses and in one evolutionary lineage of H9N2 influenza viruses of domestic poultry [37-39].
Crystallographic analysis of HA from human and H1N1 swine influenza viruses revealed hydrogen bonds between Asp225 and the galactose preceding sialic acid (2–6 bond) as well as between Asp190 and nitrogen of the amino group in glucosamine from trisaccharide 6′SLN [30].
WHAT CHANGES IN CONTEMPORARY AVIAN INFLUENZA VIRUSES MIGHT BE
SUFFICIENT FOR THEM TO OBTAIN CAPACITY FOR AIRBORNE
TRANSMISSION?
Fortunately, highly pathogenic H5N1 influenza viruses usually do not transmit from human to human. However, several cases of the disease were noted in communities when such transmission probably took place. In particular, several family members become sick in 2003, and the influenza virus isolated from them possessed a Ser227Asn mutation in the receptor-binding site and had sharply decreased affinity to Siaα2-3Gal-terminated receptors and acquired ability to bind 6′SLN [40, 41].
Stevens et al. investigated changes in receptor phenotype of H5N1 influenza viruses resulting from “classic” mutations responsible for recognition of Siaα2-6Gal by human influenza viruses [42]. It was demonstrated that the Glu190Asp substitution worsened its binding to Siaα2-3Gal, and Gly225Asp substitution did not affect it, whereas combined action of these mutations completely disrupted binding to any receptors. In other words, a mechanism employed in H1N1 viruses was unacceptable for H5N1 influenza viruses. The Gln226Leu substitution was also “inefficient” as it only lowered affinity to the receptor. However, the additional substitution Ser227Asn and especially Gly228Ser provide the virus with the capacity to bind to Siaα2-6Gal. A combination of amino acid substitutions at position 226 and 228 (as in H3N2 viruses) results in a mixed receptor phenotype having good affinity to Siaα2-6Gal-terminated receptors. It was demonstrated that clones of H5N1 influenza virus containing either Ser227Asn and Gln196Arg or Gly143Arg and Asn197Lys recognized Siaα2-6Gal. Artificial insertion of such substitutions into the HA of another H5N1 virus was also found to change receptor specificity towards recognition of Siaα2-6Gal [43].
H5N1 influenza virus isolated from humans that contained the substitutions Ala134Val and Ile151Phe possessed lowered affinity to the “avian” receptor Siaα2-3Gal [44].
However, despite the altered receptor specificity and fundamental opportunity for human-to-human transmission, none of the above-mentioned viral strains was able to spread among people. A mere alteration of receptor specificity was not enough for development of a pandemic influenza virus strain. Studies with the ferret model revealed a number of additional factors enhancing efficacy of airborne transmission. Comparing efficacy of airborne transmission for reassortant human (H3N2) and chicken (H5N1) influenza viruses demonstrated that effective transmission was provided both by external and internal viral proteins [21].
However, pandemic influenza strain can develop from reassortment, i.e. bear internal genes that have already adapted for effective transfer. Therefore, it is especially important to understand the way surface proteins in pandemic strains develop. Based on this, over recent years a number of articles have been published that examined viruses artificially generated using reverse genetics that contained internal genes derived from viruses proved to demonstrate effective transmission as well as genes encoding external proteins from avian influenza viruses [45, 46]. These studies confirmed that alteration of receptor specificity in HA is necessary but insufficient for enabling airborne transmission.
STABILITY OF INFLUENZA VIRUSES IN ACIDIC MEDIUM – AN
IMPORTANT CONDITION FOR EFFECTIVE VIRAL SPREAD
The pH value required for HA conformational transition preceding membrane fusion and entrance of viral RNA into the cytoplasm of the host cell is considered as one of the additional important conditions, whereas stability of HA in acidic medium represents the second of these conditions. It is known that highly pathogenic H5N1 influenza viruses have pH-transition higher than in human viruses, and HA is unstable at low pH values. As a result, such viruses become rapidly degraded in acidic medium of the upper airway tract, which abruptly lowers release of infectious material upon coughing and sneezing.
Imai et al. [47] and Linster et al. [48] investigated H5N1 influenza virus bearing mutations that alter receptor specificity of HA. This virus was shown to recognize Siaα2-6Gal; however, airborne transmission was negligible. By inserting additional mutations T318I or H103Y into HA that lower pH-optimal value for conformational transition and elevate its stability, the efficacy of airborne transmission in ferrets was sharply upregulated.
BALANCE OF ACTIVITIES BETWEEN HEMAGGLUTININ AND NEURAMINIDASE
MUST BE MAINTAINED FOR EFFECTIVE REPLICATION OF INFLUENZA VIRUS
The balance between activities of HA and NA has great importance for interactions of influenza virus along with receptor specificity and HA stability. In case influenza virus has a high affinity to cellular receptors and NA possesses weak capacity to degrade these receptors, then during the first life cycle virus would successfully infect cells, but the viral progeny might be poorly able to detach from the host cells, and intercellular transmission of the infectious process would be hindered. Such viruses can result in low yield and be poorly transmissible [49, 50].
Paulson et al. examined the balance between functional activities of HA and NA from swine influenza viruses, some H1N1s circulating after 2009 as well as 1918, 1957, 1968, and 2009 primary pandemic isolates. It was shown that all human viral isolates further established in evolution were characterized with approximately equal ratio of HA/NA activities, whereas for swine influenza viruses this ratio was skewed. It was concluded that “a functional match between the hemagglutinin and neuraminidase appears to be necessary for efficient transmission between humans and can be an indicator of the pandemic potential of zoonotic viruses” [51].
Due to the fact that receptor activity of HA becomes altered while entering a novel host, a restoration of balance between activities of HA and NA is one of the conditions required for development of pandemic influenza viruses. Both changes in HA and NA can facilitate solving this “task”. The sequence of NA is much more stable compared to HA, and superficial regions in HA surrounding receptor-binding site are hypervariable, which collectively underlie a two-step mutual adjustment of these influenza proteins. Enhancement of attenuation of viral binding to the target cells can be reached very quickly due to mutations that alter the protein charge. Kaverin et al. described numerous cases when the balance of activities between HA and NA was restored when disturbed in reassortant influenza viruses having low neuraminidase activity due to mutations on the top region of HA, which resulted in shifting the charge to a negative side [52-54].
Another way to restore this balance is to alter the NA. Investigation of enzymatic activity of N2 NA during evolution in human H2N2 and H3N2 influenza viruses demonstrated that capacity to cleave the Siaα2–6Gal bond was gradually upregulated [55]. NA from avian viruses poorly cleaves this bond, i.e. both HA and NA are specified for Siaα2-3Gal-receptors. Similarly, neuraminidase from the earliest human viruses isolated during 1918 and 2009 influenza pandemics was almost unable to cleave Siaα2–6Gal-bond, whereas N2 NA from H2N2 and H3N2 acquired this ability [51]. This can be interpreted as an adaptation of NA to Siaα2-6Gal-receptor specificity of HA.
HEMADSORPTION SITE OF NEURAMINIDASE AS A TYPICAL FEATURE OF AVIAN
INFLUENZA VIRUSES IS LACKING UPON TRANSITION TO MAMMALS
Upon transmission to humans, NA from avian influenza viruses can change not only due to mutations in the catalytic site. Along with the catalytic site, on the surface of each NA subunit from avian influenza virus there is an independent site able to bind to sialic acid (Fig. 1) [56] known as the hemadsorption site for its capacity to bind to red blood cells (RBCs). Six amino acids of the hemadsorption site responsible for binding to sialic acid were found to be virtually the same in nine NA antigenic subtypes (Fig. 2). Hemadsorption activity is a typical property of NA from avian influenza viruses, whereas it is lacking in human viruses.
Analyzing published amino acid sequences of NAs from viruses isolated during the 1957 influenza pandemic showed that the majority of 1957 and 1958 viruses contained mutations in one of the six amino acids mentioned above, i.e. changes within the hemadsorption site began to appear immediately after emergence of the novel pandemic influenza virus. Each of these mutations resulted in loss of hemadsorption activity typical of the avian precursor [57].
Comparison of hemadsorption activity of N1 NA from the 1918 pandemic virus and NA from the related avian viruses revealed its decrease in pandemic influenza virus [57].
Similar results were obtained for NA from pandemic 2009 influenza virus that contains NA from swine influenza viruses originating from avian H1N1 influenza virus that entered swine population and adapted approximately 35 years ago. NAs from such swine influenza viruses provide better elution of the viruses from RBCs, being less inhibited by tracheal mucins and more effectively proliferating in the cells of the human tracheobronchial epithelium compared to NA from avian viruses as well as NAs from human “epidemic” influenza viruses [58]. By comparing N1 NA from five viruses, it was demonstrated that avian influenza viruses possessed hemadsorption activity. Early “avian-like” swine influenza virus also bears this activity, but contemporary swine viruses lack it, similarly to human influenza viruses ([57], Uhlendorff, D., and Matrosovich, M. N., unpublished data).
Thus, the earliest isolates of human viruses from all four influenza pandemics were shown to lose hemadsorption activity of NA that was exhibited by the “parental” avian viruses. Most likely, these changes in NA were directly linked to adaptation of the viruses to a novel cellular receptor as well as alteration of receptor specificity in HA.
INFLUENZA PANDEMICS IN THE PAST AND FUTURE
Retrospective analysis of morbidity as well as human serum samples allows determining influenza pandemics that occurred in the distant past: in 1830 – cased by H1N1, 1847 – cased by H1N8, 1889 – cased by H3N8, 1900 – cased by H1N8 [59]. The fact that influenza pandemics have been regularly repeated over the last two centuries leaves no hope that they will not occur in the future. So far, all attempts made to predict what type of influenza virus would result in pandemic have been unsuccessful. For instance, highly pathogenic H5N1 and H7 chicken influenza viruses as well as lowly pathogenic H9N2 viruses were considered as “candidates” for influenza pandemics, as they were found to result in influenza episodes in people. Also, swine influenza viruses cause episodes in humans, but the 2009 influenza pandemic emerged totally unexpected. As a part of the preparation for potential influenza pandemics in the future, novel more universal types of vaccines as well as new anti-influenza drugs are being developed. In particular, neuraminidase inhibitors (zanamivir and oseltamivir) came into medical practice. At the same time, well-known drugs such as amantadine and rimantadine, which inhibit influenza M2 protein, have become completely ineffective, meaning that virtually all influenza viruses acquired resistance to them. Interestingly, an attempt has been made to develop a drug that might inhibit binding of influenza virus to a host cell [60]. Stringent specificity of all human influenza viruses to one receptor ligand (Siaα2-6Gal1-4GlcNAc) assures that future pandemic influenza virus will bind to it as well. On the other hand, the fact that cellular receptor and potential inhibitor match each other leaves no opportunity for influenza virus to lower affinity to inhibitor without affecting its ability to bind to host cells. Such a universal drug would be able to mitigate consequences of potential influenza pandemic in the future.
Thus, it can be said that pandemic human influenza viruses can emerge from avian progenitors under certain circumstances such as: 1) HA retargeting to recognize 2-6 sialyl-containing receptors in the human upper airway tract; 2) alteration of NA enzymatic activity necessary for maintaining functional balance with HA. Such changes require at least 1-2 mutations within conservative regions of the receptor-binding site in HA, and at least one mutation in the NA hemadsorption site. Moreover, it appears that several mutations in HA are required to enhance human-to-human airborne transmission.
This study was conducted with financial support from the Russian Foundation for Basic Research (grant No. 14-04-00547-a), the Deutsche Forschungsgemeinschaft (grant No. SFB1021), and the European Union 7th Framework Program 278433 PREDEMICS.
REFERENCES
1.Webster, R. G., Bean, W. J., Gorman, O. T.,
Chambers, T. M., and Kawaoka, Y. (1992) Evolution and ecology of
influenza A viruses, Microbiol. Rev., 56, 152-179.
2.Taubenberger, J. K., Reid, A. H., Krafft, A. E.,
Bijwaard, K. E., and Fanning, T. G. (1997) Initial genetic
characterization of the 1918 “Spanish” influenza virus,
Science, 275, 1793-1796.
3.Tumpey, T. M., Basler, C. F., Aguilar, P. V., Zeng,
H., Solorzano, A., Swayne, D. E., Cox, N. J., Katz, J. M.,
Taubenberger, J. K., Palese, P., and Garcia-Sastre, A. (2005)
Characterization of the reconstructed 1918 Spanish influenza pandemic
virus, Science, 310, 77-80.
4.Cox, N. J., and Subbarao, K. (2000) Global
epidemiology of influenza: past and present, Annu. Rev. Med.,
51, 407-421.
5.Matrosovich, M. N., Matrosovich, T. Y., Gray, T.,
Roberts, N. A., and Klenk, H. D. (2004) Neuraminidase is important for
the initiation of influenza virus infection in human airway epithelium,
J. Virol., 78, 12665-12667.
6.Paulson, J. C. (1985) Interactions of animal
viruses with cell surface receptors, in The Receptors (Conn, M.,
ed.) Vol. 2, Academic Press, Orlando, pp. 131-219.
7.Varki, A. (1997) Sialic acids as ligands in
recognition phenomena, FASEB J., 11, 248-255.
8.Rogers, G. N., and D’Souza, B. L. (1989)
Receptor-binding properties of human and animal H1 influenza virus
isolates, Virology, 173, 317-322.
9.Connor, R. J., Kawaoka, Y., Webster, R. G., and
Paulson, J. C. (1994) Receptor specificity in human, avian, and equine
H2 and H3 influenza virus isolates, Virology, 205,
17-23.
10.Matrosovich, M. N., Gambaryan, A. S., Teneberg,
S., Piskarev, V. E., Yamnikova, S. S., Lvov, D. K., Robertson, J. S.,
and Karlsson, K. A. (1997) Avian influenza A viruses differ from human
viruses by recognition of sialyloligosaccharides and gangliosides and
by a higher conservation of the HA receptor-binding site,
Virology, 233, 224-234.
11.Gambaryan, A. S., Tuzikov, A. B., Piskarev, V.
E., Yamnikova, S. S., Lvov, D. K., Robertson, J. S., Bovin, N. V., and
Matrosovich, M. N. (1997) Specification of receptor-binding phenotypes
of influenza virus isolates from different hosts using synthetic
sialylglycopolymers: non-egg-adapted human H1 and H3 influenza A and
influenza B viruses share a common high binding affinity for
6′-sialyl(N-acetyllactosamine), Virology, 232,
345-350.
12.Matrosovich, M., Tuzikov, A., Bovin, N.,
Gambaryan, A., Klimov, A., Castrucci, M. R., Donatelli, I., and
Kawaoka, Y. (2000) Early alterations of the receptor-binding properties
of H1, H2, and H3 avian influenza virus hemagglutinins after their
introduction into mammals, J. Virol., 74, 8502-8512.
13.Baum, L. G., and Paulson, J. C. (1990)
Sialyloligosaccharides of the respiratory epithelium in the selection
of human influenza virus receptor specificity, Acta Histochem.
Suppl., 40, 35-38.
14.Couceiro, J. N., Paulson, J. C., and Baum, L. G.
(1993) Influenza virus strains selectively recognize
sialyloligosaccharides on human respiratory epithelium; the role of the
host cell in selection of hemagglutinin receptor specificity, Virus
Res., 29, 155-165.
15.Subbarao, K., Klimov, A., Katz, J., Regnery, H.,
Lim, W., Hall, H., Perdue, M., Swayne, D., Bender, C., Huang, J.,
Hemphill, M., Rowe, T., Shaw, M., Xu, X. Y., Fukuda, K., and Cox, N.
(1998) Characterization of an avian influenza A (H5N1) virus isolated
from a child with a fatal respiratory illness, Science,
279, 393-396.
16.Claas, E. C., Osterhaus, A. D., Van Beek, R.,
Jong, J. C., Rimmelzwaan, G. F., Senne, D. A., Krauss, S., Shortridge,
K. F., and Webster, R. G. (1998) Human influenza A H5N1 virus related
to a highly pathogenic avian influenza virus, Lancet,
351, 472-477.
17.Matrosovich, M. N., Zhau, N., Kawaoka, Y., and
Webster, R. (1999) The surface glycoproteins of H5 influenza viruses
isolated from humans, chickens, and wild aquatic birds have
distinguishable properties, J. Virol., 73, 1146-1155.
18.Matrosovich, M. N., Matrosovich, T. Y., Gray, T.,
Roberts, N. A., and Klenk, H. D. (2004) Human and avian influenza
viruses target different cell types in cultures of human airway
epithelium, Proc. Natl. Acad. Sci. USA, 101,
4620-4624.
19.Thompson, C. I., Barclay, W. S., Zambon, M. C.,
and Pickles, R. J. (2006) Infection of human airway epithelium by human
and avian strains of influenza a virus, J. Virol., 80,
8060-8068.
20.Kogure, T., Suzuki, T., Takahashi, T., Miyamoto,
D., Hidari, K. I., Guo, C. T., Ito, T., Kawaoka, Y., and Suzuki, Y.
(2006) Human trachea primary epithelial cells express both
sialyl(alpha2-3)Gal receptor for human parainfluenza virus type 1 and
avian influenza viruses, and sialyl(alpha2-6)Gal receptor for human
influenza viruses, Glycoconj. J., 23, 101-106.
21.Maines, T. R., Chen, L. M., Matsuoka, Y., Chen,
H., Rowe, T., Ortin, J., Falcon, A., Hien, N. T., Mai, L. Q.,
Sedyaningsih, E. R., Harun, S., Tumpey, T. M., Donis, R. O., Cox, N.
J., Subbarao, K., and Katz, J. M. (2006) Lack of transmission of H5N1
avian-human reassortant influenza viruses in a ferret model, Proc.
Natl. Acad. Sci. USA, 103, 12121-12126.
22.Shinya, K., and Kawaoka, Y. (2006) Influenza
virus receptors in the human airway, Uirusu, 56,
85-89.
23.Uiprasertkul, M., Puthavathana, P., Sangsiriwut,
K., Pooruk, P., Srisook, K., Peiris, M., Nicholls, J. M.,
Chokephaibulkit, K., Vanprapar, N., and Auewarakul, P. (2005) Influenza
A H5N1 replication sites in humans, Emerg. Infect. Dis.,
11, 1036-1041.
24.Gu, J., Xie, Z., Gao, Z., Liu, J., Korteweg, C.,
Ye, J., Lau, L. T., Lu, J., Gao, Z., Zhang, B., McNutt, M. A., Lu, M.,
Anderson, V. M., Gong, E., Yu, A. C., and Lipkin, W. I. (2007) H5N1
infection of the respiratory tract and beyond: a molecular pathology
study, Lancet, 370, 1137-1145.
25.Nicholls, J. M., Chan, M. C., Chan, W. Y., Wong,
H. K., Cheung, C. Y., Kwong, D. L., Wong, M. P., Chui, W. H., Poon, L.
L., Tsao, S. W., Guan, Y., and Peiris, J. S. (2007) Tropism of avian
influenza A (H5N1) in the upper and lower respiratory tract, Nature
Med., 13, 147-149.
26.Riel, D., Munster, V. J., Wit, E., Rimmelzwaan,
G. F., Fouchier, R. A., Osterhaus, A. D., and Kuiken, T. (2006) H5N1
virus attachment to lower respiratory tract, Science,
312, 399.
27.Skehel, J. J., and Wiley, D. C. (2000) Receptor
binding and membrane fusion in virus entry: the influenza
hemagglutinin, Annu. Rev. Biochem., 69, 531-569.
28.Ha, Y., Stevens, D. I., Skehel, J. J., and Wiley,
D. C. (2001) X-ray structures of H5 avian and H9 swine hemagglutinins
bound to avian and human receptor analogs, Proc. Natl. Acad. Sci.
USA, 98, 11181-11186.
29.Ha, Y., Stevens, D. J., Skehel, J. J., and Wiley,
D. C. (2003) X-ray structure of the hemagglutinin of a potential H3
avian progenitor of the 1968 Hong Kong pandemic influenza virus,
Virology, 309, 209-218.
30.Gamblin, S. J., Haire, L. F., Russell, R. J.,
Stevens, D. J., Xiao, B., Ha, Y., Vasisht, N., Steinhauer, D. A.,
Daniels, R. S., Elliot, A., Wiley, D. C., and Skehel, J. J. (2004) The
structure and receptor binding properties of the 1918 influenza
hemagglutinin, Science, 303, 1838-1342.
31.Russell, R. J., Gamblin, S. J., Haire, L. F.,
Stevens, D. J., Xiao, B., Ha, Y., and Skehel, J. J. (2004) H1 and H7
influenza haemagglutinin structures extend a structural classification
of haemagglutinin subtypes, Virology, 325, 287-296.
32.Russell, R. J., Stevens, D. J., Haire, L. F.,
Gamblin, S. J., and Skehel, J. J. (2006) Avian and human receptor
binding by hemagglutinins of influenza A viruses, Glycoconj. J.,
23, 85-92.
33.Bateman, A. C., Busch, M. G., Karasin, A. I.,
Bovin, N., and Olsen, C. W. (2008) Amino acid 226 in the hemagglutinin
of H4N6 influenza virus determines binding affinity for alpha2,6-linked
sialic acid and infectivity levels in primary swine and human
respiratory epithelial cells, J. Virol., 82,
8204-8209.
34.Reid, A. H., Fanning, T. G., Hultin, J. V., and
Taubenberger, J. K. (1999) Origin and evolution of the 1918
“Spanish” influenza virus hemagglutinin gene, Proc.
Natl. Acad. Sci. USA, 96, 1651-1656.
35.Glaser, L., Stevens, J., Zamarin, D., Wilson, I.
A., Garcia-Sastre, A., Tumpey, T. M., Basler, C. F., Taubenberger, J.
K., and Palese, P. (2005) A single amino acid substitution in 1918
influenza virus hemagglutinin changes receptor binding specificity,
J. Virol., 79, 11533-11536.
36.Stevens, J., Blixt, O., Glaser, L., Taubenberger,
J. K., Palese, P., Paulson, J. C., and Wilso, I. A. (2006) Glycan
microarray analysis of the hemagglutinins from modern and pandemic
influenza viruses reveals different receptor specificities, J. Mol.
Biol., 355, 1143-1155.
37.Matrosovich, M., Krauss, S., and Webster, R.
(2001) H9N2 influenza A viruses from poultry in Asia have
human-virus-like receptor specificity, Virology, 281,
156-162.
38.Olsen, C. W., Carey, S., Hinshaw, L., and
Karasin, A. I. (2000) Virologic and serologic surveillance for human,
swine and avian influenza virus infections among pigs in the
north-central United States, Arch. Virol., 145,
1399-1419.
39.Liu, J., Okazaki, K., Ozaki, H., Sakoda, Y., Wu,
Q., Chen, F., and Kida, H. (2003) H9N2 influenza viruses prevalent in
poultry in China are phylogenetically distinct from A/quail/Hong
Kong/G1/97 presumed to be the donor of the internal protein genes of
the H5N1 Hong Kong/97 virus, Avian Pathol., 32,
551-560.
40.Gambaryan, A., Tuzikov, A., Pazynina, G., Bovin,
N., Balish, A., and Klimov, A. (2006) Evolution of the receptor binding
phenotype of influenza A (H5) viruses, Virology, 344,
432-348.
41.Shinya, K., Hatta, M., Yamada, S., Takada, A.,
Watanabe, S., Halfmann, P., Horimoto, T., Neumann, G., Kim, J. H., Lim,
W., Guan, Y., Peiris, M., Kiso, M., Suzuki, T., Suzuki, Y., and
Kawaoka, Y. (2005) Characterization of a human H5N1 influenza A virus
isolated in 2003, J. Virol., 79, 9926-9932.
42.Stevens, J., Blixt, O., Tumpey, T. M.,
Taubenberger, J. K., Paulson, J. C., and Wilson, I. A. (2006) Structure
and receptor specificity of the hemagglutinin from an H5N1 influenza
virus, Science, 312, 404-410.
43.Yamada, S., Suzuki, Y., Suzuki, T., Le, M. Q.,
Nidom, C. A., Sakai-Tagawa, Y., Muramoto, Y., Ito, M., Kiso, M.,
Horimoto, T., Shinya, K., Sawada, T., Kiso, M., Usui, T, Murata, T.,
Lin, Y., Hay, A., Haire, L. F., Stevens, D. J., Russell, R. J.,
Gamblin, S. J., Skehel, J. J., and Kawaoka, Y. (2006) Haemagglutinin
mutations responsible for the binding of H5N1 influenza A viruses to
human type receptors, Nature, 444, 378-382.
44.Crusat, M., Liu, J., Palma, A. S., Childs, R. A.,
Liu, Y., Wharton, S. A., Lin, Y. P., Coombs, P. J., Martin, S. R.,
Matrosovich, M., Chen, Z., Stevens, D. J., Hien, V. M., Thanh, T. T.,
le Nhu, N. T., Nguyet, L. A., do Ha, Q., van Doorn, H. R., Hien, T. T.,
Conradt, H. S., Kiso, M., Gamblin, S. J., Chai, W., Skehel, J. J., Hay,
A. J., Farrar, J., de Jong, M. D., and Feizi, T. (2013) Changes in the
hemagglutinin of H5N1 viruses during human infection –
influence on receptor binding, Virology, 447,
326-327.
45.Lu, X., Shi, Y., Zhang, W., Zhang, Y., Qi, J.,
and Gao, G. F. (2013) Structure and receptor-binding properties of an
airborne transmissible avian influenza A virus hemagglutinin H5
(VN1203mut), Protein Cell, 4, 502-511.
46.Xiong, X., Coombs, P. J., Martin, S. R., Liu, J.,
Xiao, H., McCauley, J. W., Locher, K., Walker, P. A., Collins, P. J.,
Kawaoka, Y., Skehel, J. J., and Gamblin, S. J. (2013) Receptor binding
by a ferret-transmissible H5 avian influenza virus, Nature,
497, 392-396.
47.Imai, M., Watanabe, T., Hatta, M., Das, S. C.,
Ozawa, M., Shinya, K., Zhong, G., Hanson, A., Katsura, H., Watanabe,
S., Li, C., Kawakami, E., Yamada, S., Kiso, M., Suzuki, Y., Maher, E.
A., Neumann, G., and Kawaoka, Y. (2012) Experimental adaptation of an
influenza H5 HA confers respiratory droplet transmission to a
reassortant H5 HA/H1N1 virus in ferrets, Nature, 486,
420-428.
48.Linster, M., van Boheemen, S., de Graaf, M.,
Schrauwen, E. J., Lexmond, P., Manz, B., Bestebroer, T. M., Baumann,
J., van Riel, D., Rimmelzwaan, G. F., Osterhaus, A. D., Matrosovich,
M., Fouchier, R. A., and Herfst, S. (2014) Identification,
characterization, and natural selection of mutations driving airborne
transmission of A/H5N1 virus, Cell, 157, 329-339.
49.Mitnaul, L. J., Matrosovich, M. N., Castrucci, M.
R., Tuzikov, A. B., Bovin, N. V., Kobasa, D., and Kawaoka, Y. (2000)
Balanced hemagglutinin and neuraminidase activities are critical for
efficient replication of influenza A virus, J.
Virol., 74, 6015-6020.
50.Wagner, R., Matrosovich, M. N., and Klenk, H. D.
(2002) Functional balance between haemagglutinin and neuraminidase in
influenza virus infections, Rev. Med. Virol., 12,
159-166.
51.Xu, R., Zhu, X., McBride, R., Nycholat, C. M.,
Yu, W., Paulson, J. C., and Wilson, I. A. (2012) Functional balance of
the hemagglutinin and neuraminidase activities accompanies the
emergence of the 2009 H1N1 influenza pandemic, J. Virol.,
86, 9221-9232.
52.Kaverin, N. V., Matrosovich, M. N., Gambaryan, A.
S., Rudneva, I. A., Shilov, A. A., Varich, N. L., Makarova, N. V.,
Kropotkina, E. A., and Sinitsin, B. V. (2000) Intergenic HA–NA
interactions in influenza A virus: postreassortment substitutions of
charged amino acid in the hemagglutinin of different subtypes, Virus
Res., 66, 123-129.
53.Kaverin, N. (2010) Postreassortment amino acid
substitutions in influenza A viruses, Future Microbiol.,
5, 705-715.
54.Rudneva, I. A., Timofeeva, T. A., Shilov, A. A.,
Kochergin-Nikitsky, K. S., Varich, N. L., Ilyushina, N. A., Gambaryan,
A. S., Krylov, P. S., and Kaverin, N. V. (2007) Effect of gene
constellation and postreassortment amino acid change on the phenotypic
features of H5 influenza virus reassortants, Arch. Virol.,
152, 1139-1145.
55.Baum, L. G., and Paulson, J. C. (1991) The N2
neuraminidase of human influenza virus has acquired a substrate
specificity complementary to the hemagglutinin receptor specificity,
Virology, 180, 10-15.
56.Air, G. M. (2012) Influenza neuraminidase,
Influenza Other Respir. Viruses, 6, 245-256.
57.Uhlendorff, J., Matrosovich, T., Klenk, H-D., and
Matrosovich, M. (2009) Functional significance of the hemadsorption
activity of influenza virus neuraminidase and its alteration in
pandemic viruses, Arch. Virol., 154, 945-957.
58.Gerlach, T., Kehling, L., Uhlendorff, J.,
Laukemper, V., Matrosovich, T., Czudai-Matwich, V., Schwalm, F., Klenk,
H. D., and Matrosovich, M. (2012) Characterization of the neuraminidase
of the H1N1/09 pandemic influenza virus, Vaccine, 30,
7348-7352.
59.Worobey, M., Han, G. Z., and Rambaut, A. (2014)
Genesis and pathogenesis of the 1918 pandemic H1N1 influenza A virus,
Proc. Natl. Acad. Sci. USA, 111, 8107-8112.
60.Bovin, N. V., Tuzikov, A. B., Chinarev, A. A.,
and Gambaryan, A. S. (2004) Multimeric glycotherapeutics: new paradigm,
Glycoconj. J., 21, 471-478.